WHO
Climate change: An opportunity for public health
http://www.who.int/mediacentre/commentaries/climate-change/en/
Dr Maria Neira, WHO Director, Department of Public Health, Environmental and Social Determinants of Health (PHE)
Ahead of the 2014 UN Climate Summit, the health sector added its voice, loud and clear, to growing concerns around climate change and called for swift action to mitigate the human cost of a warming world.
At a global conference convened by WHO, some 400 delegates from all regions—including senior government officials, leading scientists and development partners—agreed unanimously that climate change poses “unacceptable risks” to global public health. From water shortages to changing patterns of disease, they spoke of present-day climate trends that are endangering the health of people in their own countries.
Impact of climate change
The impact of climate change on human health is, indeed, alarming.
Around the world, variations in climate are affecting, in profoundly adverse ways, the air we breathe, the food we eat and the water we drink. We are losing our capacity to sustain human life in good health.
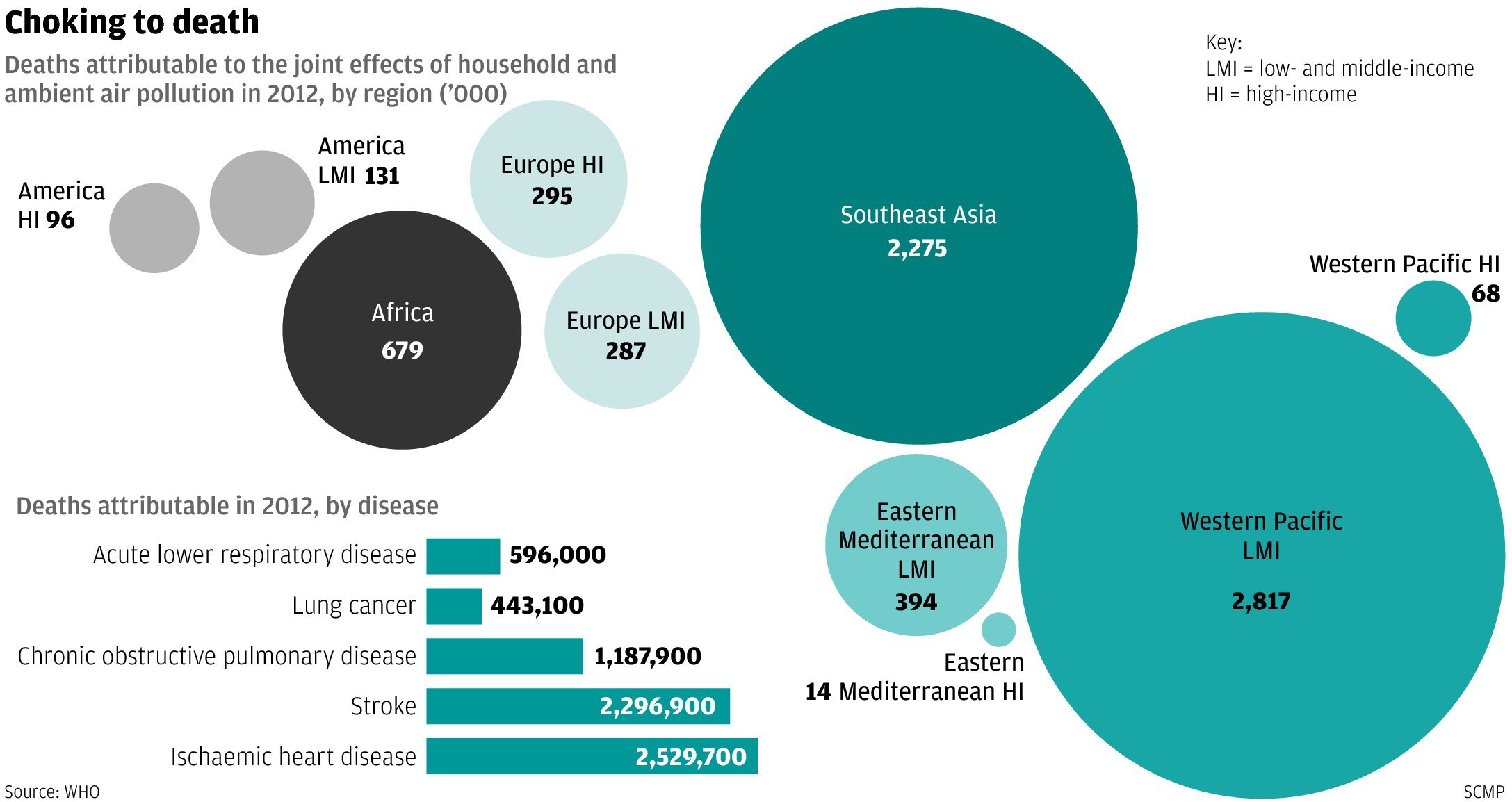
Consider air pollution, the single greatest environmental health risk we face. In 2012 alone, exposure to indoor and outdoor pollutants killed more than 7 million people—one in eight deaths worldwide.
Under-nutrition already accounts for 3 million deaths each year in the world’s poorest regions. Rising temperatures and more variable rainfall patterns are expected to reduce crop yields, further compromising food security.
Floods are increasing in frequency and intensity, creating breeding grounds for disease-carrying insects. Mosquito-borne diseases, like malaria, are particularly sensitive to changes in heat and humidity. What will happen if rising temperatures accelerate the lifecycle of the malaria parasite?
According to WHO estimates, climate change will cause an additional 250 000 deaths per year between 2030 and 2050. Most will likely perish from malaria, diarrhoea, heat exposure and under-nutrition.
Children and the elderly will be among the most vulnerable. Areas with weak health infrastructure will be least able to cope. Developing countries will be hardest hit. The health gaps we have been trying hard to close may grow even wider.
Yet against this troubling backdrop, I am optimistic.
We know that climate change mitigation can yield substantial and immediate health benefits. It is time now to translate knowledge into action.
Specific recommendations
Let me offer specific recommendations, echoing some of the views expressed at the WHO conference:
First, health sector leaders must stand hand-in-hand with climate negotiators to confront climate change. For too long, policy discussions on climate and health have been too divided. We must position health as a central pillar in the climate debate rather than an ancillary agenda.
Second, health systems must become more resilient to climate change, particularly in developing countries. Hospitals and health centres should be reinforced to withstand powerful storms, heat waves and other extreme weather events. And we must ensure that water and sanitation services continue to function under flood and drought conditions.
Third, surveillance systems for climate-sensitive infectious diseases like malaria, dengue and cholera should be fortified. Countries should make better use of early-warning information to predict the onset, intensity and duration of epidemics. Such predictions allow health officials to pre-position medicines and vaccines, which can reduce the death toll.
Fourth, we should maximize the twin benefits of climate change mitigation and improved health. Reducing emissions of short-lived climate pollutants, like black carbon and methane, would slow the rate of global warming while also saving nearly 2.5 million lives per year. Sustainable, low-carbon urban transport—such as cycling or walking as alternatives to driving cars—could lead to dramatic reductions in heart disease, stroke, breast cancer and other ailments. And there are more health benefits to be reaped from more climate-friendly housing that protects occupants from heat waves, biodiverse food production that supports healthy diets, and renewable energy systems that improve access to electricity among hundreds of millions of people in developing countries—not to mention primary health clinics where women today often give birth in the dark.
Finally, the health sector should lower its own climate footprint. Hospitals, as they operate today, are energy-intensive enterprises that contribute substantially to climate change. To reduce their environmental impact, they can adopt basic measures such as reducing toxic waste, using safer chemicals and purchasing eco-friendly products.
Cost savings
Green policies can yield substantial cost savings. In Jaipur, India, a 350-bed health facility cut its total energy bill in half between 2005 and 2008 through solar-powered water heaters and lightning. In Brazil, one efficiency project reduced the demand for electricity of a group of 101 hospitals by 1035 kilowatts at a cost savings of 25%.
Since 2007, I have described climate change as the defining issue for public health in this century. Today, I would add that it is one of the greatest opportunities we face to improve human health.
At the UN Climate Summit and beyond, I will seek support from health sector leaders and development partners to push this issue to centre stage.
Higher ambitions needed for NEC
AcidNews Jone 2015
National emission reduction commitments for 2030 should ensure achievement of the World Health Organization’s recommended air quality levels.
A coalition of environmental groups has summarised their main concerns about the proposed revision of the EU’s National Emissions Ceilings (NEC) directive, and provided inputs to the ongoing decision- making process in the European Parliament and the Council.
Every year, over 400,000 Europeans die prematurely because of air pollution. Poor air quality also makes Europeans sick and significantly reduces their quality of life, in particular in cities. Increased illness, hospital admissions, extra medication and millions of lost working days are very costly for the European Union – the health-related costs of air pollution amounted to €330–940 billion in the year 2010 alone, which is equivalent to between 3 and 9 per cent of the EU’s GDP. This includes €15 billion in direct costs from lost workdays and €4 billion from treatments of chronic bronchitis.
Air pollution also causes great harm to Europe’s ecosystems, crop yields, buildings and monuments.
Numerous studies have systematically demonstrated that the benefits of taking action to cut emissions of air pollutants outweigh the costs, in most cases by large margins.
Although environmental groups welcomed the Commission’s proposal from December 2013 to revise the National Emission Ceilings (NEC) Directive, they conclude that its ambition level does not match the scale of Europe’s air quality problems and the benefits at stake. Some of the main points of criticism are that:
• The targets, known as “Emission Reduction Commitments” (ERCs), set for 2020 have been copy-pasted from the 2012 revised Gothenburg Protocol without consideration of the potential for additional health and environmental benefits for the EU of higher ambition levels. These proposed ERCs are expected to be achieved by member states, in many cases by a wide margin, just by implementing existing legislation. In some cases, the proposed ERCs would even result in higher emissions in 2020 than are allowed under the old NEC Directive dating from 2010.
• The Commission’s proposal does not set legally binding reductions for 2025, thus risking the delay of urgently needed action until 2030.
• The proposed ERCs for 2030 are clearly not sufficient to achieve the World Health Organization’s recommended levels of air quality, which are equivalent to the EU’s long-term air quality objective as set out in the 7th Environmental Action Programme. Even after implementing the proposed 2030 ERCs, air pollution would still cause some 260,000 premature deaths every year, i.e. more than half of today’s death toll would still remain. Large areas of sensitive ecosystems would still be exposed to excessive inputs of acidifying and eutrophying air pollutants.
The European Parliament’s Rapporteur, British Conservative MEP Julie Girling, published her draft report in late March, saying that “the NEC Directive is Europe’s overarching framework piece of legislation for air quality, and without effective and implementable source legislation, member states will never meet their emission reduction targets. In other words, a further tightening of air quality standards will be redundant unless we see a clear reduction in pollution from the main sources”.
Her report recommends improvements with regard to some aspects of the Commission’s proposal, in particular the 2025 emission reduction commitments, which she proposes to make mandatory for four out of the six pollutants.
Environmental groups also welcomed her proposals to require member states to monitor the impacts of air pollution; to strengthen the role of both the Commission and the public in scrutinising national air pollution control programmes; to improve coherence between the NEC directive and the ambient air quality directive, as well as with source emission legislation; and to remove the proposed shipping flexibility.
It was noted with criticism, however, that she missed the opportunity to improve the proposal’s ambition level for 2020, 2025 and 2030, especially considering that since the Commission published its proposal nearly one and half years ago, there are new studies and developments that further strengthen the case for more ambitious air pollution reductions.
For example, recent adjustments to national emission inventories and projections by member states show more optimistic developments in air pollutant emissions in comparison with the Commission’s previous calculations (see AN 1/15, p 22).
This means that more ambitious ERCs and higher benefits could be achieved for the same initial cost.
Moreover, the European Parliamentary Research Service’s impact assessment report demonstrates that more ambition is possible and can be achieved at the same or lower cost (see AN 4/14, p 18–19). It shows that reduced consumption of polluting fuels under the EU’s new climate and energy policy agreed by the EU Council last October would decrease the need and costs for air pollution controls and make further air quality improvements significantly cheaper.
In light of the significant health, environmental and economic benefits that would result from a more ambitious NEC Directive, the environmental groups call upon the European Parliament and the Council to support:
• Significantly stricter ERCs for 2025 and 2030. The ambition level should ensure the achievement of WHO’s recommended air quality levels by 2030.
• Stricter ERCs for 2020, based on the most recent baseline figures and on a linear pathway towards the achievement of the 2025 and 2030 levels.
• Legally binding ERCs for 2025 for all pollutants covered by the directive.
• Legally binding ERCs for methane and mercury for all three target years, 2020, 2025 and 2030. (Mercury is left out of the Commission’s proposal despite being a toxic and highly transboundary pollutant causing great damage to health and ecosystems.)
• The rejection of flexibilities such as adjustment of emission inventories and offsetting of emissions between land and sea.
On 15 June, environment ministers will discuss the directive in Brussels. A vote in the Parliament’s environment committee is scheduled for 15 July, with a plenary vote in September.
Source: “NGO recommendations on the revision of the NEC directive following the publication of the rapporteur’s draft report” (13 April 2015). By the European Environmental Bureau, Transport & Environment, ClientEarth, Health and Environment Alliance and AirClim. Link: http://www.eeb.org/index.cfm/library/recommendations-following-nec-report-publication/
Air pollution costs European economies US$ 1.6 trillion a year in diseases and deaths, new WHO study says
A staggering US$ 1.6 trillion is the economic cost of the approximate 600 000 premature deaths and of the diseases caused by air pollution in the WHO European Region in 2010, according to the first-ever study of these costs conducted for the Region. The amount is nearly equivalent to one tenth of the gross domestic product (GDP) of the entire European Union in 2013.
The new study was published today by the WHO Regional Office for Europe and the Organisation for Economic Co-operation and Development (OECD) as a 3-day high-level meeting on environment and health in Europe opens. Over 200 representatives from European countries and international and nongovernmental organizations gather in Haifa, Israel, on 28–30 April 2015 to look at achievements, gaps and challenges and set future priorities.
“Curbing the health effects of air pollution pays dividends. The evidence we have provides decision-makers across the whole of government with a compelling reason to act. If different sectors come together on this, we not only save more lives but also achieve results that are worth astounding amounts of money,” says Dr Zsuzsanna Jakab, WHO Regional Director for Europe. “Cross-sectoral work is the backbone of the environment and health process, which was initiated 26 years ago, and it is even more relevant today in the discussions taking place at this meeting in Haifa.”
A ground-breaking report: economic cost of the health impact of air pollution in Europe
Economic cost of the health impact of air pollution in Europe is the first assessment of the economic burden of deaths and diseases resulting from outdoor and indoor air pollution in the 53 countries of the Region.
The economic cost of deaths alone accounts for over US$ 1.4 trillion. Adding another 10% to this, as the cost of diseases from air pollution, results in a total of almost US$ 1.6 trillion. In no less than 10 of the 53 countries of the Region, this cost is at or above 20% of national GDP (see Annex for data by country). The study uses the methodology applied in a 2014 report by OECD and makes the calculations based on the most recent economic estimates of the health impacts of air pollution.
The economic value of deaths and diseases due to air pollution – US$ 1 600 000 000 000 – corresponds to the amount societies are willing to pay to avoid these deaths and diseases with necessary interventions. In these calculations, a value is attached to each death and disease, independent of the age of the person and which varies according to the national economic context.
Air pollution: the single largest environmental health risk
Over 90% of citizens in the Region are exposed to annual levels of outdoor fine particulate matter that are above WHO’s air quality guidelines. This accounted for 482 000 premature deaths in 2012 from heart and respiratory diseases, blood vessel conditions and strokes, and lung cancer. In the same year, indoor air pollution resulted in an additional 117 200 premature deaths, five times more in low- and middle-income countries than in high-income countries.
“Reducing air pollution has become a top political priority. Air quality will be a key theme at the next Environment for Europe Ministerial Conference in Georgia in 2016”, says Mr Christian Friis Bach, Executive Secretary of the United Nations Economic Commission for Europe (UNECE). “Fifty-one countries are today finding joint solutions in the framework of the UNECE Convention on Long-range Transboundary Air Pollution. This work must be strengthened to reduce air pollution even further and extended to more countries and to other regions.”
“About 2500 people are estimated to die in Israel annually as a result of exposure to air pollutants. The main source of air pollution is transportation, mainly in major city centres,” says Mr Ofir Akunis, Deputy Minister of Environmental Protection and Member of Knesset (Parliament) for Israel. “Since 2011, the Ministry of Environmental Protection’s Clean Air Law regulates pollutants from major sources such as transport, industry and energy in accordance with the most stringent standards. The Ministry aims to use all available resources to reduce air pollution, as this means saving the lives of thousands of people, as well as billions to the Israeli economy”.
Improving environment and health in Europe: how far have we gotten?
The cost of the health impacts of air pollution is only one of many studies that will provide evidence on the environmental impacts on health to be released at the Haifa meeting.
Another new report, Improving environment and health in Europe: how far have we gotten? jointly published by WHO and UNECE, informs that one in four Europeans still falls sick or dies prematurely from environmental pollution. Data from several surveys in priority thematic areas such as water and sanitation, air quality, the day-to-day surroundings of children’s lives, chemicals and asbestos, climate change and health inequalities all show that while progress has been remarkable, it has been uneven (see Fact Sheet on the report).
Vietnamese incinerators create deadly dioxin gases
http://www.eco-business.com/news/vietnamese-incinerators-create-deadly-dioxin-gases/
Many incinerators in Viet Nam are discharging high amount of dioxins into the environment, according to a new research.
The research was carried out by the project titled Environmental Remediation in Dioxin Contaminated Hotspots in Viet Nam organised by the Office of National Steering Committee 33, the body in charge of handling the consequences of toxic chemicals used by the United States during the war in Viet Nam and the Ministry of Natural Resources and Environment (MONRE).
The research results were extracted in a report on the dioxin contamination in the environment of Viet Nam issued in November last year.
“In this report, Viet Nam admits for the first time that there’s dioxin discharged from industrial activities besides dioxin left from the war,” Le Ke Son, director of the project and former deputy head of Environment Agency under the MONRE, was quoted by Tien Phong (Vanguard) newspaper as saying.
Incinerators that burn industrial and medical waste generate most dioxin. This is shown by examination of dioxin and dioxin related compounds (DRCs) in their emission and sewage, the report said.
According to the World Health Organisation, dioxins are highly toxic and can cause reproductive and developmental problems, damage the immune system, interfere with hormones and also cause cancer.
Dioxin influences people’s health, mainly through breathing toxic air and eating polluted food. The emission of dioxin into the environment can directly affect people and animals, while the discharge of dioxin-contaminated sewage poses risk to land, water, sediment and animals.
The researchers took 18 emissions samples from medical, industrial and urban incinerators. All contained DRCs. Seven exceeding the safe limit from several to dozens of times.
Safety issue
Three out of seven samples taken from Ha Noi’s incinerators exceeded the safe limit with the one sample 16 times over the allowed level of 600 picograms toxic equivalent (TEQ) of dioxin per normal cubic metre.
Hai Duong Province had two samples of industrial waste treatment with TEQ of dioxin up to 46,800 picograms, or 81 times over the allowed level. HCM City had one sample that exceeded the permissible level by five times.
Viet Nam does not set a dioxin limit for sewage, but based on the Japanese standard of 10 picograms per normal cubic metre, HCM City has the worst dioxin pollution with three out of five samples polluted with one exceeding the limit by 5,000 times.
Two samples in Ha Noi were five and 23 times over the limit while four samples in Hai Duong Province were between three and 129 times above the permited level.
Son blamed backward technology for generating dioxin at incineration plants.
Most incinerators in Viet Nam had low capacity and few could reach the temperature needed to break down dioxin, he said. Besides, the emissions in a number of incinerators were treated by cooling, which raise concern over discharging dioxin emission into the atmosphere.
According Nguyen Huy Nga, former director of the Health Environment Management Agency under the Ministry of Health, incinerators have been banned in developed countries for many years as it pollutes the environment and poses threat to people’s health. In Viet Nam, the Ministry of Science and Technology and Ministry of Natural Resource and Environment also recommend not using incinerators.
The country now has about 400 incinerators for treating medical waste. Most have been in operation since 2000, he said.
“In 2012, MONRE set a standard for industrial incinerators. However, none of the incinerators for medical waste meet the standard,” Nga told the newspaper.
He expressed deep concern about dioxin pollution as many of the incinerators were near residential areas.
SCMP: Pollution kills 7 million people every year, says WHO report
from Lo Wei of the SCMP:
Around seven million people died in 2012 as a result of exposure to air pollution, accounting for one in eight deaths around the globe, the World Health Organisation said yesterday.
The figure has doubled over eight years. WHO officials explained that the latest estimate was more comprehensive than those in the past.
New methods were developed to measure outdoor air pollution in rural areas and more diseases like stroke and heart disease were found to be caused by air pollution, said Dr Carlos Dora, co-ordinator for interventions for healthy environments with the WHO’s Department of Public Health and Environment.
He said the figures might not show whether the problem had worsened, but he added: “The problem is at large and should be a priority.”
SCMP: A welcome move to clear the air
from the SCMP Editorial:
Smoggy days are far less common in Hong Kong than on the mainland. As we gaze above this time of year, we are more likely to see a magnificent skyline across clear blue sky than silhouettes shrouded in smog. Unfortunately, pollution knows no boundaries. Our proximity to the manufacturing powerhouse in the Pearl River Delta means we are not shielded from emissions. Experience has shown that hazardous smog does choke the city from time to time during winter. It would be wrong to assume filthy air was only confined to the mainland. The health threat of polluting air cannot be ignored.
It is good that our much-criticised air pollution index will be replaced by a new scale later this month. Introduced nearly 20 years ago, the old index shows the concentrations of pollutants in the air but tells little about the harmful effect to health. The new index is based on health risks, relating pollutant levels to short-term health risks on a scale of 1 to 10+. It also issues alerts via smartphones and provides health advice for people with various degrees of susceptibility.
Air pollution is a life-and-death issue. But the government has made little effort to put the health and economic impacts into perspective. The use of air quality standards that are less stringent than those recommended by the World Health Organisation has also led to criticism that pollution is far worse than reported. The revamp is a belated but welcome step to link pollution with public health. It provides a more meaningful reference to the community.
Officials admit that the tighter standards used in the new index might result in more days classified as bad for health. But they stress it does not necessarily mean the city’s air quality is deteriorating. Given the growing concerns about polluted air, it is not surprising that officials play down the severity of the problem. But if health alerts become more regular under the new system, the public are entitled to ask for more safeguards. Hopefully, it can instil a greater sense of urgency on the authorities to clean up the air.
23 Dec 2013
Air pollution recognized as carcinogenic, also linked to prenatal development problems
The World Health Organization (WHO) has finally reported that air pollution causes cancer: vehicle, industrial and other forms of emissions fill the air with a toxic cocktail of chemicals and particulate matter. Meanwhile, the Guardian also reports that air pollution, combined with an environment of heavy traffic, increases the likelihood of babies being born with low birthweight, which leads to other health problems. With Hong Kong suffering from both problems, the government will need to put its foot down to improve the situation if it is serious about improving its citizens’ health.

When pollution strikes hard: Air quality in March 2010 (left), compared to better days. (WSJ)
Click here for more coverage:
Will ‘measurement’ of pollutants in HK take extraterritorial sources into consideration?
Cheung Chi-fai of the SCMP reports that Hong Kong will be linking up with the World Health Organisation (WHO) to ‘develop a mechanism to measure changes in air quality and public health’ to help the city improve its environment. The plan, if it could be called one at all at this time, is extremely vague, but even if it becomes the best-laid of plans, it would run into a fundamental problem: the basis of the study is an investigation about the city’s clean air policies, but some of the worst air pollutants come from outside the city’s jurisdiction. For example, ocean-going vessels passing through Hong Kong’s nearby shipping channels use bunker fuels with 2.75 to 4% sulphur content, significantly higher than the 0.005ppm(0.0000005%) of Euro5 diesel fuel; prevailing easterly winds blows sulphur compounds and respirable suspended particles (RSP) into Hong Kong, a situation worsened by the density of urban structures that helps to trap air particles within its confines. The many incinerators on the Shenzhen side of the border also figures to be a major factor in Hong Kong’s air quality.
This ‘plan’ would need more serious thinking if it intends to be anywhere near producing true analysis of Hong Kong’s air quality.